Coming home after surgery should feel like a relief. But for most people, it’s actually when the hard part begins. You’re in pain. Simple things like getting out of bed or walking to the kitchen feel impossible. Your body won’t cooperate the way it used to. And suddenly you’re wondering how you’re going to manage basic daily tasks that you never had to think about before.
I’ve seen this struggle countless times with families here in Chicago. The surgery itself is over, but now you’re facing weeks or even months of recovery. You can’t bend the way you need to. You can’t lift things. You get tired just standing up. And maybe you live alone, or your family works full time and can’t be there during the day.
This is exactly why home care after surgery exists. Not because you’re weak or incapable, but because recovering from surgery is genuinely difficult and sometimes you need an extra set of hands to get through it safely. Let me walk you through what this actually looks like and how it helps people manage the real physical challenges that come after surgery.
Understanding Physical Limitations After Surgery
Your body has been through trauma. That’s really what surgery is when you think about it. Even though it’s controlled and medically necessary, your body still has to heal from being cut open, having things moved around or removed, and then being stitched back together.
Pain is the first thing that hits you. Not just soreness, but actual pain that makes you catch your breath when you move the wrong way. Your incision hurts. The muscles around it are tender. And this pain doesn’t just make you uncomfortable. It stops you from doing things. You literally can’t move in certain ways because it hurts too much.
Then there’s the weakness. This surprised me the first time I saw it up close with my own father after his knee surgery. Here was a man who’d worked construction for 30 years, and he couldn’t walk from the bedroom to the bathroom without needing to rest. Surgery drains your energy in ways you don’t expect. Your body is using everything it has to heal itself, which leaves very little for anything else.
Movement becomes a puzzle you have to solve. After hip surgery, you can’t bend past a certain angle. After abdominal surgery, you can’t twist or reach up. After shoulder surgery, forget about lifting your arm above your head. These aren’t just recommendations. These are real limitations based on what your body can physically handle while tissues are healing.
Balance gets wonky too. Maybe it’s the pain medication making you dizzy. Maybe it’s a weakness affecting your stability. Or maybe you’ve just been off your feet for a few days and your body forgot how to balance properly. Whatever the reason, you feel unsteady. And that makes every step scary because you know falling could really hurt you or damage the surgical repair.
The fatigue is relentless. You sleep eight or ten hours and wake up exhausted. You do one small task and need a nap. This isn’t laziness. Your body is working incredibly hard behind the scenes to heal wounds, fight off infection, and rebuild tissue. That work is invisible but it’s absolutely exhausting.
What Home Care After Surgery Looks Like
When people hear home care, they sometimes picture a nurse in white scrubs hovering over them all day. That’s not really how it works.
A caregiver comes to your house for whatever amount of time you need them. Maybe it’s three hours in the morning to help you shower, get dressed, and eat breakfast. Maybe it’s eight hour shifts so someone is there most of the day. For people who really need it, especially right after major surgery, a caregiver might stay overnight too.
What do they actually do? The real, everyday stuff that becomes difficult when you’re recovering.
They help you get out of bed without falling or twisting wrong. They walk with you to the bathroom and wait outside in case you need help. They assist with showering, which is trickier than it sounds when you can’t bend over to wash your feet or reach behind you, and when you have to keep incisions dry.
Getting dressed becomes a whole ordeal after surgery. You can’t pull your pants up while standing on one leg after knee surgery. You can’t reach behind your back after shoulder surgery. Your caregiver helps you figure out how to get clothes on without violating any of your movement restrictions.
Food is another big one. You need to eat well to heal, but standing in the kitchen cooking takes energy you don’t have. Your caregiver prepares meals, makes sure you’re drinking enough water, and probably nags you a bit about eating even when you don’t feel hungry.
They also keep track of all your medications. After surgery, you might be taking pain pills, antibiotics, blood thinners, and your regular prescriptions. It’s easy to lose track of what you took when. Your caregiver manages all of this so you don’t accidentally skip doses or double up.
And honestly, one of the most valuable things they provide is just being there. Recovery can feel lonely and scary. Having someone to talk to, someone who can call for help if something goes wrong, someone who notices if you’re not yourself today… that matters more than people realize.
How Post Operative Care Supports Daily Movement
Here’s what most people don’t understand until they’ve been through it: moving after surgery is both essential and terrifying. You have to move to prevent complications like blood clots. But moving also hurts and puts you at risk of falling.
Post operative care helps you navigate this impossible balance.
Getting in and out of bed is the first challenge every single day. After hip surgery, you have to learn a whole new technique. You can’t just swing your legs over the side like you used to. There are rules about angles and which direction you can turn. A caregiver physically helps you move and reminds you of the technique every single time until it becomes automatic. Because trust me, at 3am when you need the bathroom and you’re half asleep, you will forget the right way to move.
Walking is crucial but also when most falls happen. You’re weak, possibly dizzy from medication, and dealing with pain that throws off your balance. Your caregiver walks right next to you, ready to catch you if you start to go down. They make sure you’re using your walker correctly. They help you set realistic goals, like walking to the end of the hallway today and maybe to the living room tomorrow.
The bathroom is honestly where a lot of people need the most help. Sitting down on the toilet and standing back up requires core strength and leg strength you might not have right now. The bathroom floor is usually hard tile, which makes falls extra dangerous. Caregivers help with these transfers and often suggest equipment like raised toilet seats that make things safer and easier.
Stairs can be a nightmare. Even just two or three steps to get into your house become a major obstacle. Some people avoid stairs completely for the first few weeks, which is fine if you can set up everything you need on one floor. But if you need to navigate stairs, your caregiver helps you do it safely, one step at a time, using the railing, no rushing.
The goal of all this help isn’t to keep you dependent. It’s the opposite actually. It’s to help you move as much as you safely can, because movement is what rebuilds your strength and gets you back to independence faster.
Role of Physical Therapy in Recovery at Home
Physical therapy sounds intimidating, but it’s really just exercises designed specifically for what your body needs right now.
A physical therapist comes to your house and works with you. They look at how you’re moving, test your strength and range of motion, and figure out what you need to work on. Then they give you exercises that target exactly those areas.
These aren’t gym workouts. We’re talking about really simple movements. After knee surgery, you might do leg lifts while lying in bed. After shoulder surgery, maybe you use a cane to help lift your arm gradually higher. The exercises look almost too easy to matter, but they’re perfectly calibrated to challenge your healing body without overdoing it.
The therapist shows you how to do each exercise correctly. They watch your form and correct it if you’re compensating in weird ways that could cause new problems. They push you just enough to make progress without pushing so hard that you hurt yourself.
Then they leave, and you’re supposed to do these exercises multiple times a day on your own. And this is where having a home caregiver becomes really valuable. Because let’s be honest, when you’re tired and sore, it’s really easy to think I’ll skip the exercises today. A caregiver reminds you, encourages you, and sometimes even helps hold resistance bands or count repetitions. They keep you accountable when your motivation disappears.
The progress feels painfully slow at first. You gain maybe five degrees of bend in your knee this week. Next week maybe you can lift your arm two inches higher. It doesn’t feel like much day to day. But compare where you are after four weeks to where you started, and the difference is actually dramatic.
Home based therapy has some real advantages. You don’t have to get dressed and drive somewhere when you’re exhausted and in pain. The therapist sees your actual home and can suggest modifications, like moving that throw rug that could trip you. You practice real activities in your real environment, like going up your actual stairs or getting in your actual shower.
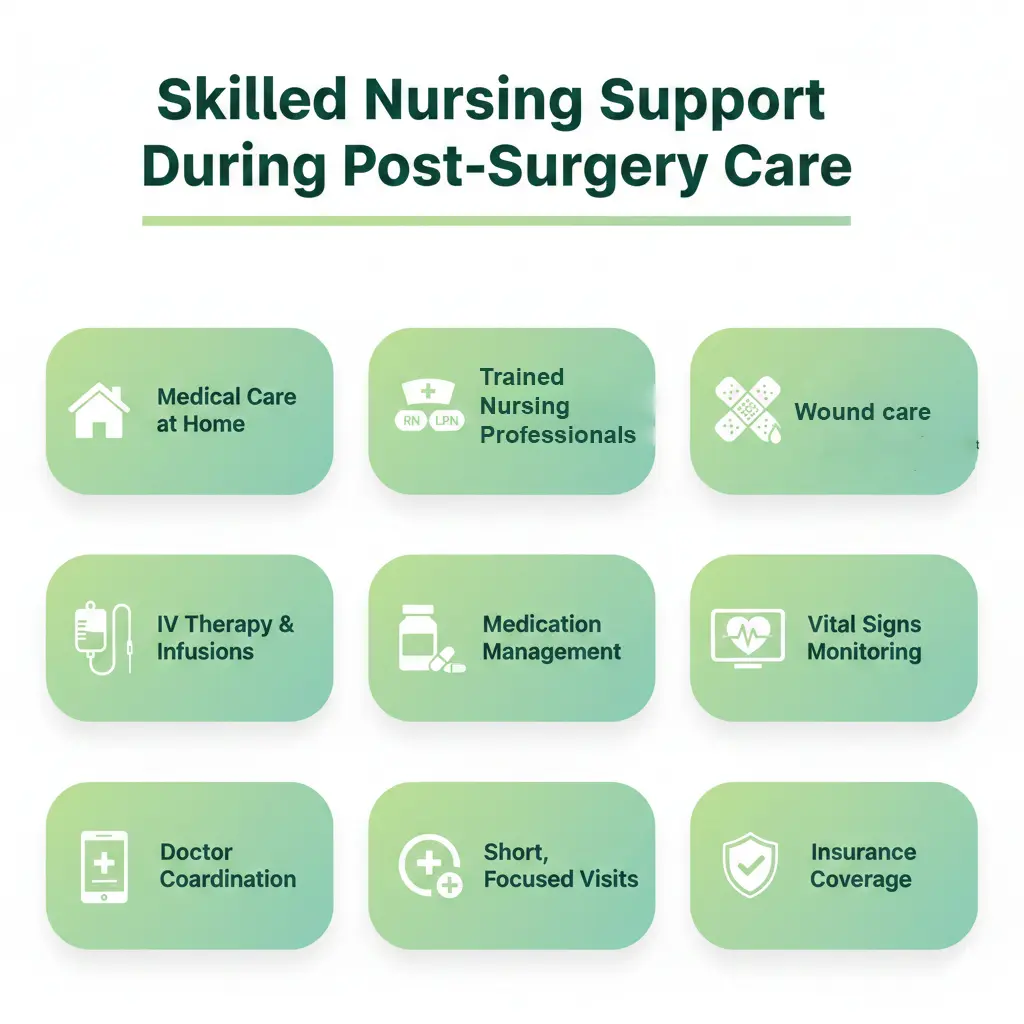
Skilled Nursing Support During Post Surgery Care
Some people need more than just help with daily activities. They need actual medical care at home. That’s when skilled nursing comes into the picture.
A registered nurse or licensed practical nurse comes to your house to handle medical tasks that regular caregivers aren’t trained for.
Wound care is probably the most common reason for skilled nursing. Some surgical incisions are complicated. You might have drains coming out that need to be emptied and measured. You might have a wound vac attached. The dressing needs to be changed using sterile technique. And the whole time, the nurse is watching carefully for any signs of infection that need immediate attention.
Some people come home still needing IV antibiotics or other infusions. Managing an IV line isn’t something just anyone can do. The nurse administers the medication properly, checks the IV site, and monitors you for any reactions.
Managing multiple medications gets complicated fast. You’re taking pain pills every four hours, antibiotics three times a day, blood thinners that interact with other drugs, plus all your regular medications. A skilled nurse reviews everything, watches for dangerous interactions, and makes sure you understand what each medication does.
They also monitor your vital signs regularly. They check your blood pressure, heart rate, temperature, and oxygen levels. They know what’s normal for you and what might signal a problem developing. If they see something concerning, they contact your doctor right away instead of waiting for it to become an emergency.
Skilled nursing visits are usually shorter and less frequent than regular caregiver visits. The nurse might come once or twice a day for specific medical tasks, while a home health aide is there for longer periods helping with daily activities.
Insurance often covers skilled nursing when your doctor prescribes it as medically necessary. This makes it accessible for many people who need this level of care during recovery.
Why Recovery at Home Is Often Easier Than Facility Care
When doctors give you the option, most people choose to recover at home rather than go to a rehabilitation facility. And there are good reasons for that preference.
Your own home is just more comfortable. Your own bed, your own pillow, your own temperature settings. These things matter when you’re trying to heal. You’re not adjusting to a new environment while your body is already stressed from surgery.
Sleep is so much better at home. Hospitals and rehab facilities are noisy. Someone comes in to check vital signs every few hours. You hear other patients, alarms going off, staff talking in hallways. At home, you can actually sleep when your body needs rest. And sleep is when a lot of healing happens.
The infection risk is lower at home too. Healthcare facilities are clean, but they’re also full of sick people and drug resistant bacteria. At home, you’re only exposed to your own household germs. This matters a lot when your immune system is focused on healing your incision.
Being around family helps emotionally in ways that are hard to measure but definitely real. Your spouse can sit with you without waiting for visiting hours. Your grandkids can stop by and cheer you up. You can wear your own clothes, eat food you actually like, and watch your own TV. These small comforts reduce stress, and less stress supports better healing.
You also get more personalized attention at home. Your caregiver focuses entirely on you, not on five other patients down the hall. Meals can be made to your actual preferences. The daily schedule can flex around when you feel good versus when you feel terrible.
Cost matters too, though people don’t always want to admit it. Home care has expenses for sure, but it’s often less than an extended stay in a rehab facility. And many insurance plans cover at least some home health services.
This doesn’t mean everyone should recover at home. Some surgeries are complex enough that you really do need the intensive monitoring of a facility, at least for a while. But for many people, home is absolutely the better choice if you can arrange proper support.
Managing Pain and Preventing Complications at Home
Pain management after surgery is about more than just popping pills, though medication is definitely part of it.
Your doctor prescribes pain medication based on your surgery and pain level. Taking it on schedule works way better than waiting until you’re miserable and then trying to catch up. A caregiver helps by keeping track of doses and reminding you when it’s time for the next one, even if you don’t feel like you need it yet. Staying ahead of pain is easier than fighting your way back from severe pain.
Ice helps a lot in those first few days. It reduces swelling and numbs the area enough to give you relief. Your caregiver can apply ice packs at the right intervals and make sure they’re wrapped so you don’t damage your skin.
Positioning yourself properly makes a bigger difference than you’d think. Elevating a swollen leg, supporting your back with pillows, finding the right angle for sitting… all of this affects your pain level. A caregiver helps you get positioned comfortably and readjusts pillows when you shift around.
Preventing falls becomes critical during recovery. You’re weaker than usual, possibly dizzy from medication, dealing with pain that affects your balance. Falls can be devastating. Caregivers help prevent them in practical ways. They clear tripping hazards like loose rugs and clutter. They make sure lights are on before you move around. They grab bars get installed in the bathroom if needed. You wear real shoes with grip instead of slippery socks.
Blood clots are a serious risk after surgery, especially if you’ve been less mobile. Simple things help prevent them. Ankle pumps, leg exercises, walking short distances several times a day. Compression stockings might be part of your prevention plan too. A caregiver makes sure you’re doing these things even when you’re tired and don’t feel like it.
Constipation is miserable and really common after surgery. Pain medications slow everything down. So does being less active. Your caregiver makes sure you’re drinking enough water, eating fiber when your doctor says it’s okay, and taking stool softeners if prescribed. They also notice if constipation is becoming a real problem before it turns into an emergency.
Watching for infection is an ongoing job. Your caregiver looks at your incision every day. Is it redder than yesterday? Is there new swelling? Any drainage? Do you feel warmer than usual? Catching infections early makes them so much easier to treat.
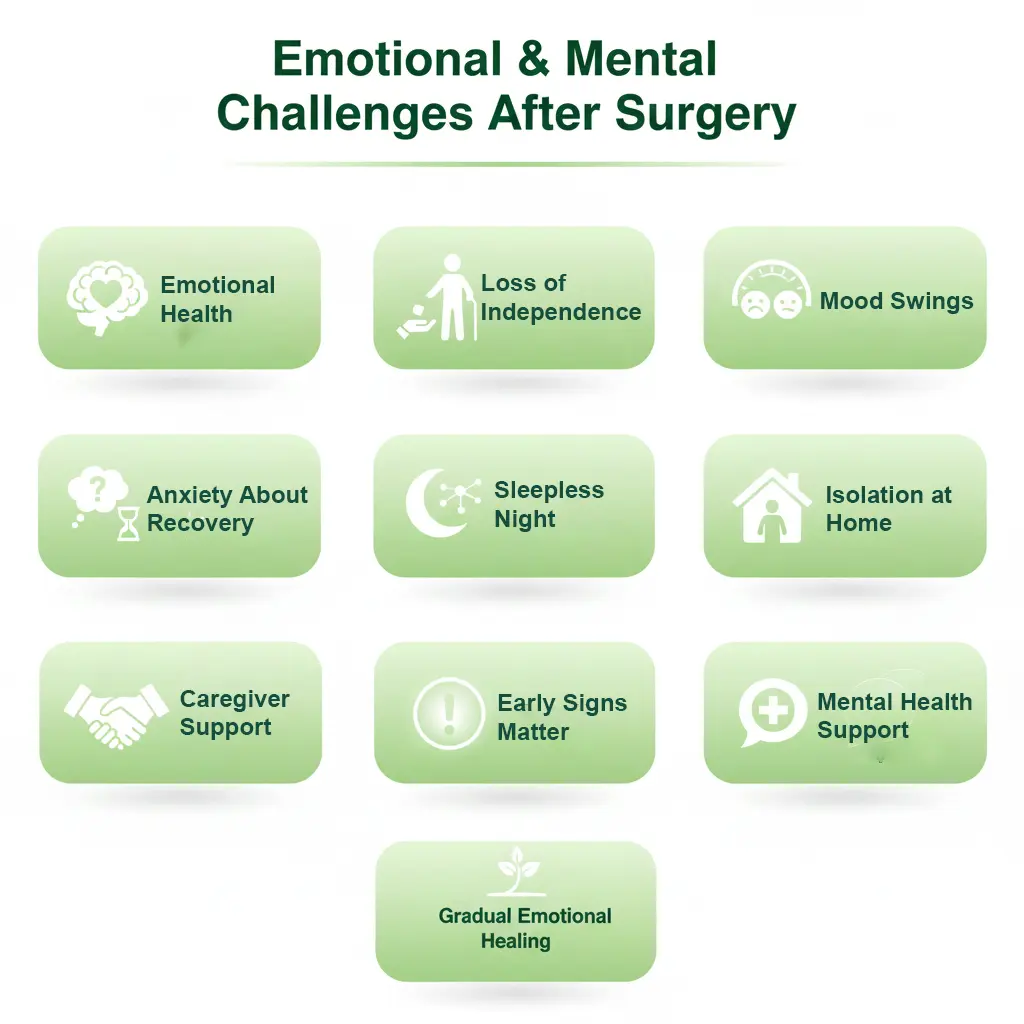
Emotional and Mental Challenges After Surgery
The physical stuff is obvious. Everyone expects pain and weakness after surgery. But the emotional impact catches people completely off guard.
Frustration builds when you can’t do simple things for yourself. Needing help to shower or get dressed can feel embarrassing, even humiliating, even though you logically know it’s temporary. People who’ve been independent their whole lives really struggle with this. I’ve seen grown men nearly in tears because they couldn’t put their own socks on.
Your mood swings in ways you don’t recognize. Part of it is pain wearing you down. Part of it is lack of good sleep. Some pain medications mess with your mood directly. Add in worry about whether you’ll fully recover, and it’s no wonder people feel emotional during this time.
Anxiety about the future keeps you awake at night. Will you get your full range of motion back? How long is this really going to take? What if something goes wrong? What if you’re not healing right? These thoughts spiral, especially when you’re lying in bed at 2am in pain.
The isolation gets to people more than they expect. You can’t go to work. You can’t go out with friends. You’re stuck at home day after day. Friends visit at first, but then life goes on for everyone else while you’re still trapped in recovery mode.
This is where a caregiver provides support that goes way beyond physical help. They’re someone to talk to when the walls are closing in. They listen when you need to vent your frustration. They’ve seen other people go through this and can reassure you that what you’re feeling is completely normal.
A good caregiver notices when you’re having a particularly rough day emotionally. They can let family know you need extra support. They make sure you’re not spending every single day isolated and alone with your anxious thoughts.
Sometimes the emotional stuff needs professional help. If you’re noticing real depression that isn’t lifting, persistent anxiety, or thoughts that worry you, tell your doctor. There’s no shame in needing mental health support during recovery. It’s part of healthcare, not a character flaw.
The good news is that emotional struggles usually improve as physical recovery progresses. As your pain decreases and you regain independence, your mood typically lifts too. But during those hard early weeks, having someone there who understands makes a tremendous difference.
When Families in Chicago Should Consider Home Care After Surgery
Not everyone needs professional home care, but a lot of Chicago families find it makes recovery safer and way less stressful.
Age is one obvious factor. If you’re a senior living alone, the risks during recovery are just higher. Falls are more dangerous. Complications can develop faster. Confusion from medications is more common. Having someone there provides safety and peace of mind for you and your family.
The type of surgery matters a lot. Major operations like hip replacement, heart surgery, spinal procedures, abdominal surgeries… these involve serious limitations. You’re going to struggle with basic tasks for weeks. These situations almost always benefit from home care after surgery.
Living alone is a big consideration. If there’s no one else in the house, who helps you in the middle of the night? Who’s there during the day if something goes wrong? Even people who live with family might need more help than their loved ones can realistically provide, especially if everyone works full time.
Existing health conditions complicate recovery. If you’re managing diabetes or heart disease on top of surgical recovery, it’s a lot to handle. A trained caregiver helps coordinate everything.
If you were already having mobility issues before surgery, recovery is going to be even harder. Professional help ensures you don’t fall and hurt yourself while you’re even weaker than usual.
Family availability is just practical. Your adult kids might want to help, but they have jobs and their own families. They live in different parts of Chicago or different states entirely. They can’t take three weeks off work to provide 24/7 care. Professional home care fills that gap without destroying everyone’s life.
A lot of Chicago families wait until after surgery to realize they need help. But planning ahead works so much better. You can interview caregivers when you’re not exhausted and in pain. You can understand costs and arrange schedules ahead of time. You can have everything set up so support starts the day you come home.
Many insurance plans cover some home health services if your doctor prescribes them as medically necessary. Medicare covers skilled nursing and therapy under certain conditions. It’s worth checking your benefits before surgery.
The point isn’t to take away your independence. It’s to provide support during a temporary period when your body genuinely needs help to heal properly.

Common Mistakes During Post Surgery Recovery
People make understandable mistakes during recovery. You’re in pain, exhausted, and just want to feel normal again. But these mistakes can really set you back.
Doing too much too soon is the biggest one. You have one good day and think you’re better than you are. You try to carry a heavy bag of groceries. You bend over to pick something up off the floor. You walk farther than you should. Then you pay for it with increased pain and swelling, and you’ve possibly damaged healing tissue.
Skipping medications or exercises happens when you start feeling better. You figure you don’t need the pain medication anymore, so you stop taking it. Or the physical therapy exercises feel boring and pointless, so you skip a few days. Both decisions slow your recovery significantly.
Not asking for help comes from pride. You don’t want to be a burden. You don’t want to seem weak. So you attempt things alone that aren’t safe yet. You don’t mention symptoms that worry you. You push through severe pain instead of adjusting your approach or asking for assistance.
Ignoring warning signs is dangerous. Increased pain, new swelling, redness, fever. These might indicate a complication. But you tell yourself it’s probably nothing and decide to wait and see. By the time you finally call the doctor, a minor issue has become a serious problem.
Eating poorly slows healing. You don’t feel hungry, or cooking seems impossible, so you skip meals or live on crackers. Your body needs good nutrition to heal. It needs protein to rebuild tissue, vitamins for immune function, calories for energy. Poor nutrition directly affects how fast and how well you recover.
Not following movement restrictions can undo the surgery. Your surgeon tells you not to bend past 90 degrees or not to lift more than five pounds for specific reasons. Violating these restrictions because they’re inconvenient can damage the surgical repair and require additional surgery to fix.
Home care helps prevent a lot of these mistakes. A caregiver keeps you on track with medications and exercises. They notice warning signs and make sure you report them. They help with tasks so you don’t overdo it. They ensure you’re eating properly and following restrictions.
Recovery requires patience that’s really hard to maintain when you’re frustrated and uncomfortable. But rushing it almost always backfires.
Frequently Asked Questions
How long do most people need home care after surgery?
It really depends on what kind of surgery you had and how your body heals. Some people need help for just a week or two. Others need it for a month or more. Your surgeon should give you an estimate for your specific situation, but be flexible because everyone heals differently.
Does Medicare cover home health care after surgery?
Medicare covers skilled nursing care and physical therapy at home if your doctor says you need it and you meet certain requirements. Regular home care assistance for daily activities might not be covered. You’ll need to check with your specific Medicare plan about what your benefits include.
Can family members handle all the care needed after surgery?
Sometimes yes, but it’s exhausting work that requires being available around the clock. Many families find that getting professional help for at least part of each day makes recovery easier and less stressful for everyone.
What’s the difference between a home health aide and a skilled nurse?
A home health aide helps with daily activities like bathing, dressing, and meals. A skilled nurse provides medical care like wound care, IV medications, and monitoring vital signs. Some people need both during recovery.
How do I find reliable home care in Chicago?
Ask your surgeon or the hospital discharge planner for recommendations. They usually have relationships with home care agencies they trust. You can also check online reviews and verify credentials. If possible, interview caregivers before your surgery.
What if I can’t afford home care?
Talk to the hospital social worker about options. Some insurance covers more than you might think. Family and friends might be able to help in shifts. Community organizations sometimes offer support services. There are usually more options available than people initially realize.
When should I call my doctor during home recovery?
Call for fever, increased pain that medication doesn’t help, signs of infection at your incision, chest pain, trouble breathing, leg swelling with pain, confusion, or anything that feels seriously wrong. It’s always better to call and be told everything’s fine than to ignore a real problem.
Conclusion
Recovering from surgery is hard. There’s really no way around that. The physical limitations you’re dealing with aren’t weaknesses. They’re your body’s normal response to trauma and the healing process.
Home care after surgery gives you support during this difficult temporary period. It keeps you safe. It helps you follow your recovery plan even when you’re exhausted and discouraged. It allows you to heal at home in comfort instead of in a facility.
For families in Chicago dealing with surgical recovery, getting professional home care often makes the difference between struggling through it and actually healing well. It reduces stress for everyone and improves outcomes.
Yes, recovery takes time. Yes, there will be frustrating days and setbacks. But with proper support, most people do heal and get back to their normal lives. Give yourself permission to accept help right now. It’s not weakness or giving up independence. It’s being smart about giving your body what it needs to heal properly. You’re going to get through this. Having someone there to help just makes the journey less scary and more manageable. Read More

